Mesothelioma Treatment Options
Depending on where the cancer is, the type of mesothelioma, your doctor will have a range of treatment options for you. The best treatment for you may include surgery, chemotherapy, radiation therapy or a combination of these treatments.
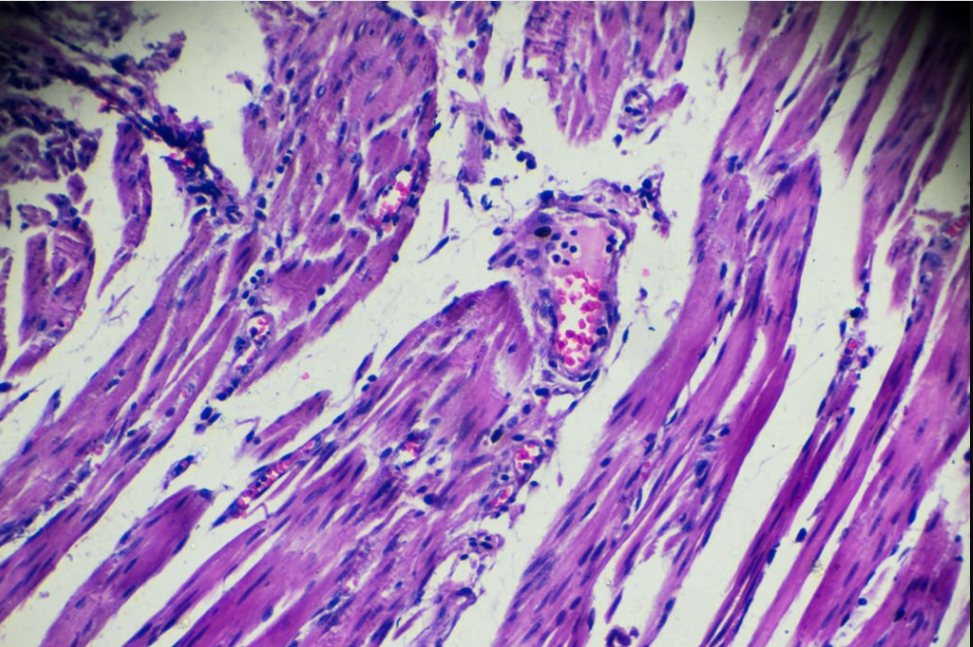
Mesothelioma can develop in either the pleura, the tissue that covers and protects your lungs or the peritoneum, the lining of your abdomen. Your doctor will need to take a tissue sample from your chest to diagnose the type of mesothelioma you have.
Chemotherapy
Chemotherapy is a treatment option that uses medicines to attack cancer cells. It may be used alone or with other treatments. It usually involves several sessions with rest periods in between.
Your doctor will work with other healthcare professionals to determine a treatment plan that will fit your needs and lifestyle. They will also help you choose the best dosage of drugs to use.
Drugs may be given orally, as an injection, or by using a device called a port or pump. Your doctor will give you instructions about how to prepare for the drugs and what to do if you have any problems.
Many people have a hard time getting through the side effects of chemotherapy, including nausea and vomiting. Your doctor may provide special supplements to reduce the risk of these problems. You can also talk to a counselor for support.
Your chemotherapy treatment will be based on lab tests that show the extent of the disease and your personal health. Your doctors will tell you if you need a higher or lower dose of the drug than the recommended amount to treat the cancer effectively.
Some chemotherapy drugs are given in the blood through a tube in your arm or leg (intravenous). Other drugs are given by mouth, as a pill, liquid, or cream.
You will need to take your medications on schedule. Make sure you have plenty of fluids and a healthy diet to keep your body healthy and able to absorb the medicines.
If you have a job, ask your doctor how chemotherapy might affect your work and if it’s a good idea to change your hours. If it is, make arrangements with your employer to work remotely or take time off on treatment days.
Another option is biologic therapy, which boosts your immune system to fight the cancer. It is still in clinical trials and may be a possible treatment option for people with mesothelioma who cannot have surgery.
Your oncologist will decide the best course of treatment based on your age, overall health, and the type of mesothelioma you have. They will try to find the best combination of drugs that will kill the cancer cells while causing the least side effects.
Radiation
Radiation therapy, also called x-ray or photon therapy, can be an effective treatment option for people with pleural mesothelioma. It uses high-energy beams of radiation to kill cancer cells without damaging nearby healthy tissue. It is usually given as a single treatment, but may be given more than once if your doctor thinks that it will help you live longer and relieve symptoms.
When you receive radiation therapy, a machine called a linac creates a special, powerful beam of x-ray or photon energy that focuses on the tumor. The computer software on the linac adjusts the size and shape of the beam to target the tumor while avoiding healthy tissue around it.
The type of radiation that is used depends on the stage and type of mesothelioma. Ionizing radiation, which is the most common type of radiation, can destroy cells by knocking electrons off atoms. It can also damage the structure of DNA molecules in cells.
It can also cause other health effects that do not appear until many years after an exposure. These delayed effects include a higher risk of developing certain types of cancer, like breast cancer and leukemia.
If you have a recurrence of mesothelioma, a new type of radiation therapy called PET-guided dose escalation tomotherapy can be used. It is based on the idea that mesothelioma cells have receptors for radioactive materials, so ionizing radiation can reach them and destroy them.
This method of delivering radiation can be more precise than a regular x-ray or photon beam, which makes it safer for some patients and can allow higher doses of radiation to be delivered more effectively. It is often given after an extrapleural pneumonectomy, where 1 of the 2 lungs is removed (see Surgery).
Because mesothelioma cells are so sensitive to radiation, it’s important that a large dose is delivered to the tumor with each session of radiation. This is why it’s usually given every weekday for several weeks. You can wear a form-fitting support or a plastic mesh mask to keep you still during treatment.
Some of the most common side effects from radiation therapy include skin changes, nausea and vomiting, fatigue, pain in the mouth and throat, and dry mouth or thick saliva. Depending on the dose of radiation, these effects can last for days or months. Some rare side effects are more serious and can be permanent, including lung damage.
Surgery
Surgery can be a powerful tool for treating mesothelioma. It can reduce pain, relieve symptoms and extend your life expectancy. It can also help your doctor make the right diagnosis and plan the best treatment for you.
There are many different types of surgeries for mesothelioma, and it is important to talk to your healthcare team about all your options so you can choose the right one for you. If you decide that surgery is not the best option for you, then you have the right to say “no” and be treated with respect.
Your medical team will make sure you are healthy enough for surgery before your procedure. This includes a preop checkup with your GP or other specialist, testing for conditions such as diabetes or heart disease and checking for any signs of infection. If you are having a procedure that involves removing your lungs, a chest X-ray or CT scan may be needed to find the best site for the operation.
Once the operation is complete, you will be moved to a room where you will be monitored by nurses. They will be sure to give you any painkillers or other medicines you need to stay comfortable.
The surgery will usually take about an hour or less, and you will likely feel groggy and drowsy when you wake up. Your doctor or nurse will then tell you what to expect next. You may need to go home the same day, or you might be transferred to another hospital room if your procedure is an overnight stay.
Infections are the most common type of surgery-related complication, and they can be devastating. They can cause redness and pain at the surgery site, drainage or fever.
To prevent infections, healthcare providers should follow the WHO’s Safe Surgery Saves Lives campaign, which sets out four key areas of surgical care that can significantly improve patient safety. These areas include surgical site infection prevention, safe anaesthesia and a safe surgical team.
Surgery for mesothelioma can be a complex and potentially dangerous procedure, so it’s important to work with a team of experts who know what they are doing. The team may include a thoracic (chest) surgeon, a respiratory physician and a medical oncologist. They will work with you and your loved ones to develop an effective treatment plan.
Pleurodesis
Pleurodesis is a treatment that drains air or fluid build-up in the pleural space, which is the space between the lungs and chest wall lining. It is usually done by a surgeon who puts a tube (chest drain) into the lung. The tube is then filled with a medicine that irritates the lining of the lung, stopping the buildup of air or fluid.
Doctors will tell you what medicines to stop taking a week or so before the procedure, and how long you should expect to be in hospital. They will also give you anaesthetic and painkillers to take during the surgery.
The operation usually takes about 1.5 hours and is done under general anaesthetic. The doctor will put the tube into your lung and fill it with a medicine called doxycycline or talc powder that will stick to the lung.
They will then use a small tool to remove the tube. This will allow the fluid to drain out of your chest and you will recover in hospital for around 3-5 days.
Some patients may be given painkillers to help with the pain after the operation. Occasionally, a small stitch will be used to close the insertion site.
The main indication for pleurodesis is malignant pleural effusion (MPE). However, it can be applied in patients with other underlying diseases as well. Among the most common malignant pleural effusions are lung cancer, breast cancer and lymphoma.
Other conditions that can result in a build-up of fluid in the pleural space include recurrent pneumothorax and recurrent pleural effusions. The former is a symptom that is difficult to treat and can cause breathing difficulties.
A number of surgical procedures can be used to treat recurrent pneumothorax and pleural effusions. These include extrapleural pneumonectomy (EPP) and pleurectomy with decortication (P/D).
Alternatively, you can have a procedure that drains the fluid from your chest into a shunt. This will drain the fluid into the abdomen and it is more likely to be absorbed by your body.
The results of a study suggest that the talc pleurodesis technique is an effective and safe method for treating recurrent pleural effusions. It is also less invasive than some surgical techniques and has an overall survival rate of 14 months.